Address
304 North Cardinal St.
Dorchester Center, MA 02124
Work Hours
Monday to Friday: 7AM - 7PM
Weekend: 10AM - 5PM
Address
304 North Cardinal St.
Dorchester Center, MA 02124
Work Hours
Monday to Friday: 7AM - 7PM
Weekend: 10AM - 5PM
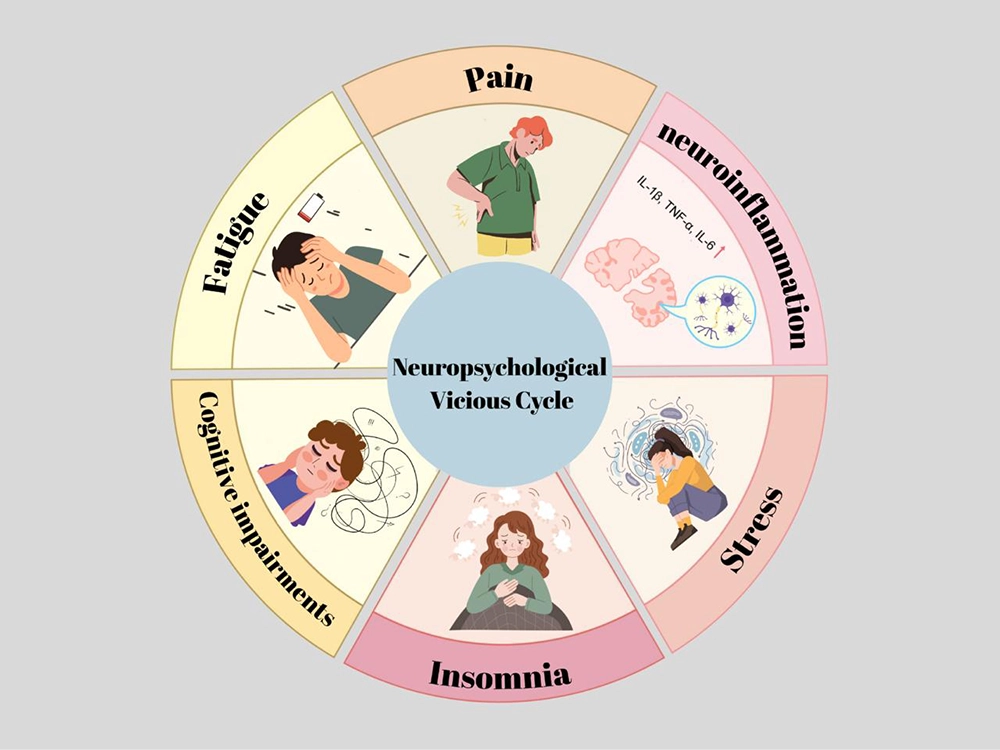
Chronic Sleep Deprivation and Stress Trigger Inflammatory Response in the Brain
Sleep deprivation increases the levels of proinflammatory cytokines such as IL-6 and IL-1β, as well as C-reactive protein (CRP). During deep sleep, cerebrospinal fluid circulation accelerates, facilitating the clearance of toxins (e.g., beta-amyloid). However, sleep deprivation impairs this cleansing mechanism, thereby increasing inflammation. Experimental studies have shown that 24 hours of sleep deprivation causes a significant rise in inflammatory markers. In neuroimmune disorders such as MOGAD, involvement of sleep centers may directly increase inflammation and exacerbate disease severity.
⸻
Neuroinflammation and Pain
• Chronic neuroinflammation induces microglial cell activation, sensitizing pain transmission pathways and causing central sensitization. This intensifies the transmission of pain signals from the spinal cord to the brain, resulting in hyperalgesia (a lowered pain threshold).
• Cytokines and chemokines (e.g., TNF-α, IL-1β) released from glial cells and neurons render neurons hyperactive, thereby increasing pain through chronic inflammation. As the level of neuroinflammation rises, pain intensity also increases—explaining why pain is a common symptom in MOGAD and NMOSD patients.
• Studies have reported increased rates of depression and fatigue in NMOSD/MOGAD patients associated with inflammation; pain, depression, and fatigue are interrelated symptoms that reinforce each other.
⸻
Neuropathic Pain and Fatigue
• Severe chronic neuropathic pain is associated with increasing fatigue throughout the day. One study found a strong correlation between pain severity and fatigue scores.
• Over time, rising pain leads to a subsequent increase in fatigue. A cross-lagged panel analysis showed that each increase in pain severity predicted a rise in fatigue in the next assessment (β≈0.55 and β≈0.36; p<0.05).
• Persistent pain depletes both physical and mental energy reserves, leading to chronic fatigue. In MOGAD, patients experiencing pain reported poor sleep quality and elevated anxiety-depression scores, all of which intensified their sense of fatigue.
⸻
Fatigue and Insomnia
• Increased fatigue can further disrupt sleep patterns. When pain and fatigue co-occur, nighttime awakenings increase, and restorative sleep becomes ineffective. In MOGAD patients, neuropathic pain has been shown to significantly reduce sleep quality, triggering new episodes of insomnia or sleep disorders.
• The relationship between pain and sleep is bidirectional: A poor night’s sleep exacerbates pain, and intensified pain disrupts sleep again. Within this vicious cycle, fatigue and reduced resilience gradually become chronic.
• As a result, patients increasingly experience a state of being “tired but awake,” waking up unrefreshed. As anxiety and physical discomfort reinforce insomnia, the cycle persists.
⸻
Stress, Depression, and Other Factors
• Chronic stress and psychological pressure trigger inflammation. Long-term stress disrupts the HPA axis, raising levels of cytokines such as IL-6 and TNF-α. This increase in inflammation adversely affects nervous system function and raises the risk of depression.
• Depression and anxiety deepen the cycle. In MOGAD, depression frequently co-occurs with pain and fatigue, and inflammation reinforces this relationship. Depressive mood increases pain perception while also worsening fatigue, concentration problems, and sleep disturbances.
• Cognitive dysfunctions are a reflection of inflammation. Chronic inflammation particularly impairs higher-order functions such as memory and attention. For example, a PET study in patients with chronic fatigue syndrome revealed that inflammation in the amygdala and thalamus correlates with the severity of cognitive impairment. This cognitive decline may further contribute to stress and insomnia in patients.
These interactions demonstrate how, in MOGAD patients, symptoms can mutually reinforce one another—both psychologically and physiologically.
At MOGAD Solidarity, we place strong emphasis on patient mental health.
Raising awareness on this topic is one of our core missions, and your support in sharing this message is deeply valuable to us.
References:
https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2022.945661/full
https://www.frontiersin.org/journals/behavioral-neuroscience/articles/10.3389/fnbeh.2022.945661/full
https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2020.00778/full
https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2023.1130989/full
https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2020.00778/full